Moving forward from a benefit denial can be complex. Discover how to launch an appeal to turn the decision in your favor.
By: Maria Williams
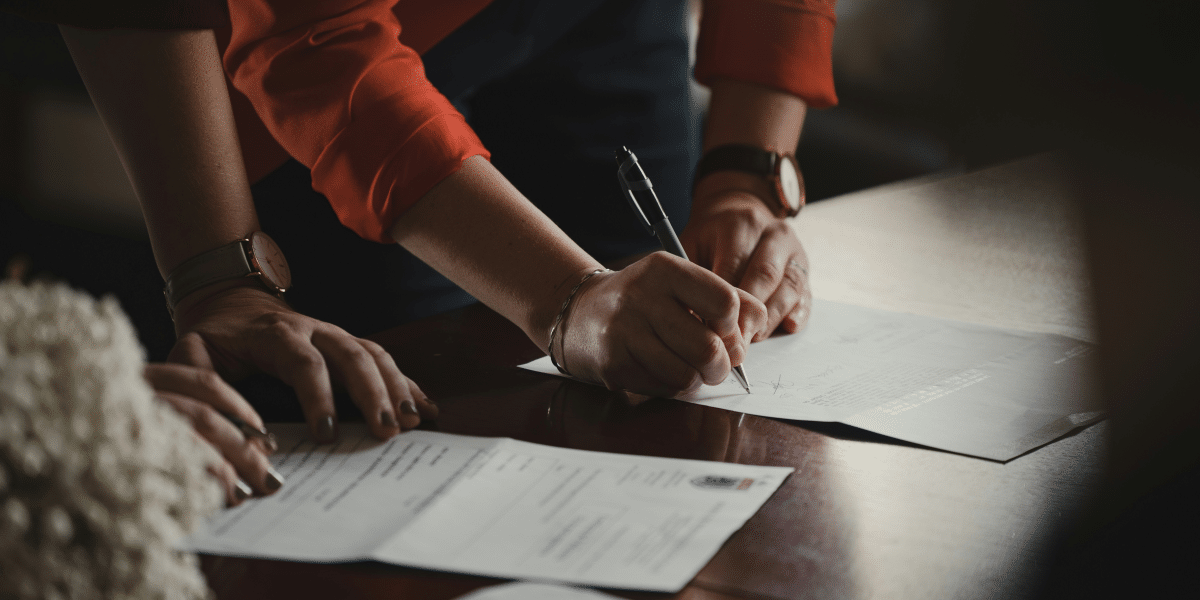
Lodging a claim is the first step in accessing private or state-backed benefits. While the requirements could vary depending on the claim, it’s crucial to know which documents to submit for a seamless process.
However, doing so doesn’t always guarantee approval. Your application can still be denied for various reasons. For example, over three million disabled worker applications were received at the State Determination Services (DDS) and field offices in 2023, according to the Security Services Administration. Of these, only 44.99% of DDS and 29.49% of field office claims were awarded.
The good thing is that a benefit denial isn’t the end of the world. You have the right to appeal the decision, and this guide will equip you with the knowledge to fight for the coverage you deserve.
Understanding the reasons for benefit denials
There are several reasons for benefit denial, depending on your insurance type and policy coverage. Claim rejections are often centered on these aspects:
Incomplete or inaccurate information
Insurance coverage doesn’t automatically result in repayments. Whether accessing medical or disability benefits, your claim should be backed by comprehensive medical information, which includes:
- Your medical history
- Physician or specialists’ diagnosis and prognosis about your medical condition, including the functional restrictions and limitations caused by your disability
- Historical records of laboratory and imaging tests to back up health claims
- Your doctor’s treatment plan
Note that the pre-existing conditions not covered under the policy might undermine your eligibility. Similarly, the insurance company may require you to ask for additional records to prove your medical claims or disability and assess its severity.
Failure to meet the eligibility criteria
It’s estimated that 14 million Americans receive disability benefits monthly. Still, many claimants are rejected because of these issues:
- Non-inclusion: If your injury or illness isn’t included on the covered conditions and impairments list, prepare to fight harder to get your claim approved. The same holds if your physician and facilities aren’t included in the insurer’s network.
- The income threshold for disability: Your current income generation capabilities will also be put into question. For Social Security Disability Insurance (SSDI), for instance, you have to prove that you’re earning below the Substantial Gainful Activity (SGA) of USD$ 1,550 for non-blind and USD$ 2,590 for blind individuals.
Preparing for an appeal
Employers typically offer disability benefits, while individuals can also purchase their own. Private and state insurance companies have different timelines and processes for an appeal, which generally involves the following steps:
Seeking expert help
When filing an appeal, seeking professional assistance is often the best course of action. However, knowing how to choose the right lawyer is crucial to navigating the process effectively. So, how do you go about it? Here are some valuable tips:
- Work with someone who handles issues like yours
- Examine their track record and success rates
- Find out what their clients have to say about them.
Experienced claims attorneys can help you dissect and understand your policy better and provide strategies that truly work. Having them by your side can make it much easier for you to achieve your desired outcomes.
Reviewing the denial letter
A benefit denial letter states the reasons for the rejection. It outlines the steps you must follow if you want to be reconsidered. Moving forward, study potential errors—whether on your part or the payer’s. For example, an applicant may meet the medical requirements for disability. Still, they may need to establish the non-medical requirements for approval.
Understanding your rights and deadlines
Applicants have the right to ask for reconsideration, regardless of which regulatory or state laws cover your benefit provider. Most private disability insurance companies impose a 180-day limit for disability claim review requests. Meanwhile, most health insurance denials can be appealed within 60 days after receiving the notice. Check your plan to determine the processes and timelines for your policy.
The appeal processes
Appeals for declined disability claims under the Social Security Administration (SSA) will be re-screened by a DDS staff who wasn’t involved in the first evaluation for questions about disability qualifications.
You’ll receive a letter regarding the status of their consideration request or your scheduled hearing before the administrative law judge, who’ll go through all of the previous and additional documents submitted. If the judge decides unfavorably, you can elevate your concern to the Appeals Council, who will decide whether to approve or decline your review request.
On the other hand, the Employee Retirement Income Security Act (ERISA) is a federal law that governs many employer-sponsored benefit plans, including disability insurance. So, if ERISA governs your disability insurance plan, the appeals process may involve additional steps. For instance, if the internal review upholds the denial, ERISA allows you to request an external review by a neutral third party, often a medical professional specializing in your condition.
As a last resort, you may have the right to file a lawsuit in federal court under ERISA. This is a complex legal process, and consulting with an attorney specializing in ERISA disability law is highly recommended.
Tips for a successful appeal
While timelines matter, making reasonable arguments backed by evidence is equally important. To increase the chances of reversing a claim denial, you must:
- Highlight any errors or inconsistencies in the denial decision
- Provide clear and concise arguments to address the reason for rejection
- Submit additional supporting evidence
- Demonstrate medical necessity or eligibility
Hiring a legal counsel is just one piece of the puzzle. It would help to work closely with healthcare professionals and your insurance provider to ensure a robust defense.
Conclusion
Benefit payments are lifelines for employees who can no longer work temporarily or permanently because of sickness or disability. It replaces the income a team member would have earned before being incapacitated. However, the claims process can be complex. You must stay persistent and keep tabs on valuable information from your healthcare and insurance providers. In most cases, seeking advice from a legal counsel is your best option—whether or not you plan to take the company to court.
Published by: Martin De Juan