By: Elena Mart
Dean Gregorie was sixteen years old when his mother first noticed something was off, a small hump between his shoulders, just below his neck. It was subtle but unmistakable. When combined with weight gain and a rounded face, she feared the worst. The symptoms pointed toward a rare hormonal disorder she had read about in a textbook: Cushing’s disease. However, when they went to their family physician, he dismissed her fears.
“Teenagers gain weight,” he explained.
What followed was a 20-year odyssey of misdiagnoses, suffering, and unspoken agony. Dean’s story is not just a story of medical malpractice; it’s a chilling tableau of what occurs when the patient falls through the cracks. And yet, it’s also a powerful testament to hope, family, and the struggle to be recognized.
The Disease No One Saw
Cushing’s disease strikes just 2 or 3 individuals per million annually. Triggered by a tiny tumor in the pituitary gland that causes excess cortisol production, it ravages almost every part of the body. The signs are unambiguous: truncal obesity, moon face, thinning skin, poor wound healing, hypertension, and purple striae. And yet, for decades, none of Dean’s physicians connected the dots.
They provided diet programs. They suggested exercise routines. They gave him physical therapy. Even as bright purple striations carved across Dean’s abdomen and his blood pressure soared, doctors continued to dismiss it as merely a result of poor lifestyle choices.
“The hump got bigger, fatigue worsened, and bruises became more frequent,” recalls Dean. “Each time, they told me to eat better and lose weight. I started feeling like it was my fault.”
The Family Who Wouldn’t Remain Silent
All along, his parents, Henry and Helen, would not give up. Helen read medical journals, textbooks, and online forums. Henry, a pharmacist by training, read endocrinology textbooks at the kitchen table.
“We were watching our son slowly disappear,” Helen said. “It felt like no one was listening.”
One evening, in a quiet yet emotional moment, Helen remembered the first time she confronted Dean’s primary care doctor and asked why he had refused to run basic cortisol tests. His response? “Cushing’s is rare. It’s probably just obesity.”
Their story echoes that of countless patients with rare diseases, where visibility often determines the quality of care. According to the NIH, it takes an average of 4.8 years and visits to five different doctors to get a diagnosis for a rare disease. For Dean, it took more than fifty doctors over the course of two decades.
A Crisis Years in the Making
By 2013, the physical and emotional toll had become unbearable. Dean collapsed at the hospital’s front doors from diabetic ketoacidosis—a life-threatening complication—and was rushed to the ICU, gasping for air. His parents got the call no family ever wants to receive.
“We’ll be there in the morning,” Helen told the nurse through tears. “Tell him to hold on.”
He did.
An endocrinologist was brought onto his care team, but only to address the immediate crisis. Despite a clear pattern of symptoms and signs his mother had long recognized, not a single test for Cushing’s disease was ordered. The deeper cause remained ignored.
What could have been a turning point became just another missed opportunity.
In 2017, Dean experienced an explosive worsening of symptoms. At work, a fall ripped through his paper-thin skin, leaving an avulsion as large as a man’s hand.
By 2018, the infections began—cellulitis, again and again, followed by a cascade of mysterious ailments. At that point, he was under the care of a second endocrinologist, as well as multiple primary care physicians. Still, no one ran the tests his mother had pleaded for all those years ago.
Then, in November 2019, a new primary care physician finally took a comprehensive look at the whole pattern, every symptom, every unexplained shift in Dean’s health. He ordered a series of tests. And finally, after more than two decades of silent suffering, the diagnosis came: Cushing’s disease.
The tumor was removed in 2020.
Reclaiming Life One Day at a Time
Recovery did not bring relief; it brought reckoning. Dean awoke from surgery, not renewed but ravaged. The tumor was gone, but so was the natural cortisol his body had long overproduced. Now, cortisol had to be replaced artificially. His strength vanished. His stamina collapsed. And his nights became battlegrounds of sleepless hours and aching uncertainty.
Days stretched into weeks. Weeks into months. The smallest movements—showering, walking, standing upright—required a level of grit he hadn’t known he possessed. And then came the back pain: unrelenting, relentless, the long-term result of vertebral damage left to fester for years without proper treatment.
“There wasn’t a morning I woke up feeling better,” Dean recalls. “There was just a morning I woke up and decided to try again.”
That choice to try again, to endure again, became its own kind of progress. The path wasn’t upward but forward. And even now, years later, he remains on constant medical watch. But for the first time, the question is no longer what’s wrong with me; it’s how I live with what I now know.
Beyond the Diagnosis

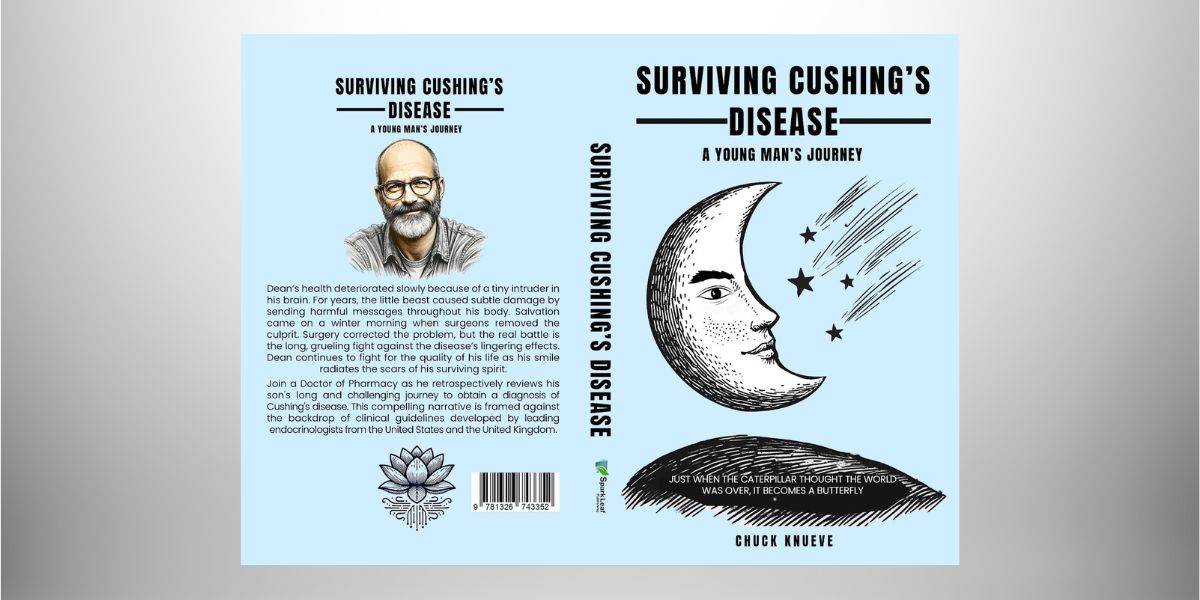
This book, Surviving Cushing’s Disease: A Young Man’s Journey, marks the author’s first step into advocacy for orphan and rare diseases. Dean’s story speaks not just to those still searching for answers but also to the medical professionals whose decisions hold the weight of human lives.
Disclaimer: This article is based on the personal experience of Dean Gregorie and does not constitute medical advice. The information presented is for informational purposes only and should not be used to diagnose or treat any medical condition. If you or someone you know is experiencing symptoms similar to those described, please consult a healthcare professional.