Image Commercially Licensed From: Unsplash
Prostatitis, an inflammation or infection of the prostate gland, often presents a unique set of diagnostic and management complexities for healthcare professionals. This inflammatory condition, often causing pain in the groin, painful urination, and other urinary issues, affects individuals across a wide age range. Understanding the diagnostic process and identifying the appropriate first-line antibiotic therapy is imperative in managing and potentially resolving prostatitis while considering its physical and psychological impact on affected individuals.
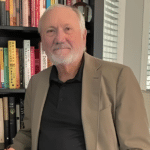
Dr. Philippe Smith, a distinguished family practitioner and the VP of the regional doctors association AMOSO (L’Association des médecins Omnipraticiens du Sud-Ouest) has been a pivotal figure in progressing our understanding of prostatitis. His exemplary academic journey began with an honors degree in Cell and Molecular Biology from Concordia University, leading to a Medical Doctorate from the University of Montreal. Dr. Smith, whose career has spanned roles at Clinique Le Trait D’Union and Anna Laberge Hospital, and substantial contributions to the Fédération des médecins omnipraticiens (FMOQ), brings forth his expertise and comprehensive understanding of diagnosing and treating prostatitis. His publications on the subject and hands-on experience dealing with numerous complex cases provide crucial insights into the nuanced approaches to the effective management of prostatitis.
Diagnostic Challenges
Diagnosing prostatitis accurately can be intricate due to its diverse clinical manifestations and the existence of various subtypes, namely acute bacterial prostatitis, chronic bacterial prostatitis, chronic pelvic pain syndrome, and asymptomatic inflammatory prostatitis.
“Effectively diagnosing prostatitis requires recognizing its varied presentations and distinguishing its subtypes to ensure precise management and treatment,” says Dr. Philippe Smith.
Clinical Assessment: Initial evaluation typically involves a thorough clinical history and physical examination, focusing on urinary, bowel, sexual, and pain symptoms. DRE (Digital Rectal Examination), a standard procedure, allows healthcare providers to assess the size, shape, and consistency of the prostate.
Laboratory Testing: Following clinical assessment, laboratory testing, involving urinalysis, urine culture, and sometimes blood tests, are performed to identify any signs of infection or inflammation.
Imaging: In some cases, imaging studies like ultrasounds or CT scans may be utilized to rule out other potential causes of the symptoms.
Symptom Score Indexes: Instruments like the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) can be employed to quantify symptom severity and monitor treatment progress.
Navigating through these stages can be complex as overlapping symptoms with other urological conditions, such as benign prostatic hyperplasia (BPH) and interstitial cystitis, can mislead the diagnostic trajectory. Additionally, non-bacterial prostatitis, which does not involve a bacterial infection, tends to be more prevalent but also more challenging to diagnose and manage, further complicating the process.
“Untangling the complexity of prostatitis diagnoses demands a meticulous approach, given its multifaceted presentations and the nuanced differences among its subtypes,” says Dr. Philippe Smith. “Integrating a thorough clinical assessment with laboratory testing, strategic use of imaging, and the insightful application of symptom score indexes is pivotal in steering accurate diagnoses and tailoring an effective management and treatment strategy for each patient.”
First-Round Antibiotic Treatment
Once a diagnosis of bacterial prostatitis is established, immediate intervention with antibiotic therapy is critical to managing the condition effectively and preventing complications such as bacteremia or prostatic abscess. The choice of antibiotic is typically guided by several key factors, including the patient’s age, medical history, type of prostatitis, and the likely causative bacteria.
Acute Bacterial Prostatitis: This form, often caused by Escherichia coli or other gram-negative bacteria, demands prompt treatment. A fluoroquinolone, like ciprofloxacin, or a third-generation cephalosporin is commonly used initially, especially in outpatient settings. The duration of therapy is typically 2-4 weeks, depending on patient response and severity.
Chronic Bacterial Prostatitis: Management of this type can be more complex due to the need for prolonged antibiotic courses and the risk of recurrence. Fluoroquinolones are commonly used due to their excellent prostate penetration, with treatment durations extending to several weeks. Alternative options may include trimethoprim-sulfamethoxazole or tetracyclines if the patient cannot tolerate fluoroquinolones.
It is crucial to note that antibiotic choice should ideally be informed by urine culture and sensitivity results to ensure effective eradication of the causative organism. In the absence of culture data, empiric therapy should be guided by local antimicrobial resistance patterns and modified accordingly once culture results are available.
“Initiating prompt and suitable antibiotic therapy in bacterial prostatitis is paramount, considering the acute nature of the condition and potential complications,” says Dr. Philippe Smith. “Adhering to a strategic approach, which incorporates the patient’s specific medical contexts and adapts to culture and sensitivity data, is instrumental in not only managing the present infection but also in circumventing recurrence and ensuring the comprehensive well-being of the patient.”
Contending with Antibiotic Resistance
The growing phenomenon of antibiotic resistance, particularly in the context of recurrent or chronic bacterial prostatitis, presents an additional layer of complexity. Multi-drug resistant organisms necessitate alternative therapeutic approaches, sometimes involving combination antibiotic therapy or the use of less commonly utilized agents, which may have additional side-effect profiles that require monitoring.
The trajectory from recognizing potential prostatitis symptoms to accurately diagnosing and initiating first-round antibiotic therapy is characterized by multiple intersections of clinical judgment, differential diagnostics, and strategic therapeutic planning. Attuning to the diagnostic challenges and being adept with the arsenal of first-line antibiotic choices while also factoring in the emerging concern of antibiotic resistance ensures a robust and patient-centric approach to managing prostatitis.
Addressing prostatitis demands an insightful appreciation of its varied presentations and a conscientious approach to diagnosis and treatment to ameliorate immediate symptoms and enhance long-term outcomes and quality of life for affected individuals.
About Dr. Philippe Smith
Dr. Philippe Smith, VP of the regional doctors association AMOSO (L’Association des médecins Omnipraticiens du Sud-Ouest), carries a legacy of excellence in his medical career. Armed with an honors degree in Cell and Molecular Biology from Concordia University and a prestigious Medical Doctorate from the University of Montreal, he has demonstrated unwavering commitment to the field. His residency at Maisonneuve Rosemont Hospital sculpted his medical acumen, leading him to his current roles at Clinique Le Trait D’Union and Anna Laberge Hospital.